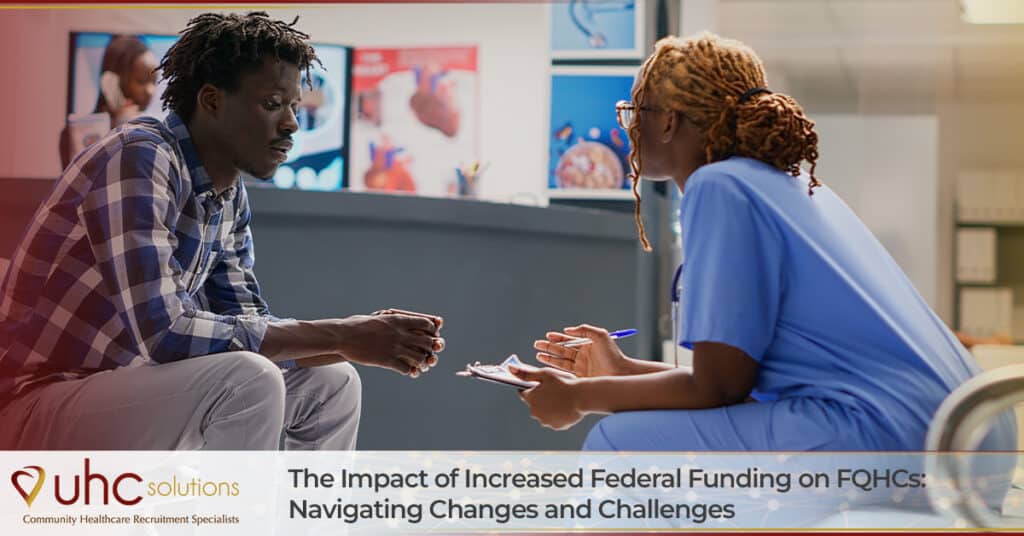
In recent years, Federally Qualified Health Centers (FQHCs) and other National Association of Community Health Centers (NACHC) organizations have been crucial in delivering affordable and comprehensive healthcare services to underserved populations across the United States. Today, one in every 11 people in the United States rely on these critical infrastructures for healthcare. But the landscape for these essential health providers is evolving, with increased attention and support from federal funding sources. This surge in financial backing brings both opportunities and challenges as FQHCs strive to meet the growing demands of their communities.
The ACA of Yesterday and Today: FQHC Funding Changes
From 2011 to 2015, the Patient Protection and Affordable Care Act (ACA) provided an increase of $11 billion in new funding for community healthcare providers. The backbone of FQHCs lies in their mission to provide accessible, high-quality healthcare to individuals regardless of their ability to pay. With the injection of increased federal funding, these health centers had the opportunity to expand their reach and impact. One significant advantage of increased federal funding is enhancing infrastructure in terms of physical facilities and technological capabilities. Upgrading medical equipment, expanding clinic spaces, and adopting advanced health information systems can contribute to a more efficient and effective healthcare delivery system.
Increased federal funding also allows FQHCs to attract and retain skilled healthcare professionals. Competitive salaries, training programs, and professional development opportunities become more feasible, addressing the workforce shortages in underserved areas. It ensures that communities relying on FQHCs receive not only accessible but top-notch healthcare services.
However, as FQHCs navigate changes from increased federal funding, they also encounter several challenges. One is that changes in federal policies also mean evolving budgets and compliance requirements, such as the November 2023 final ruling from the Centers for Medicare and Medicaid Services (CMS) that will significantly impact community healthcare providers. For example, rural healthcare patients will benefit from service expansions for billable services to CMS, such as remote physiologic and therapeutic monitoring, mental health, and addiction treatment, and more.
At the same time, The Commonwealth Fund points out, “Inflation-adjusted federal funding for centers has decreased over time, while the number of clinics, total patients served, and operating costs have all increased, stretching limited funds even further.” Given that community health centers rely heavily on Medicaid reimbursements (approximately 44% of all funding to these organizations) and that these resources have remained relatively flat over the years, it is a challenge. What other challenges do FQHCs face in the future?
FQHC Fiscal Challenges
One of the primary concerns is the need for strategic financial management. While additional funding is a boon, FQHCs must allocate resources judiciously to sustain long-term operations. Implementing robust financial management practices will ensure any influx of funding translates into lasting improvements in patient care.
Another challenge is the demand for expanded services. With increased federal funding, FQHCs may experience a surge in patient visits, necessitating an expansion of services to meet the community’s growing healthcare needs. This pressure requires careful planning to ensure that the quality of care remains consistent despite increased patient volumes. FQHCs must invest in scalable solutions and innovative care delivery models to maintain accessibility without compromising service quality.
Technology integration poses both an opportunity and a challenge. While federal funding can facilitate the adoption of advanced healthcare technologies, the implementation process can be complex. FQHCs must balance embracing innovation and ensuring that technology enhances, rather than hinders, the patient’s experience. Training staff, updating infrastructure, and maintaining cybersecurity become critical components of this technological transformation.
What’s Next for FQHCs?
The impact of federal funding on FQHCs is multifaceted, bringing both opportunities and challenges. While the additional resources empower health centers to improve, these organizations are vulnerable to changes in federal policy that could jeopardize care delivered to underserved populations.
UHC Solutions remains an advocate and strong partner of community healthcare organizations. We offer turnkey recruiting of clinical and administrative staff that frees up overburdened HR teams in these critical institutions. Call on us to find out how we can help.